Peer-reviewed paper published in Climate.
Abstract: During the 2022 summer, Europe experienced heatwaves with record temperatures, and a study has argued that they caused about 62,000 deaths between 30 May and 4 September. The total number of excess deaths during the same period was about 137,000, indicating that the heatwaves were a substantial contributor. Not ruling out that explanation entirely, this paper argues that it was unlikely a strong cause. First, if the heatwaves were a strong cause of numerous deaths, one would assume that the older and deprived were relatively likely to die. However, during the 2022 summer heatwaves in England, which were claimed to have caused about 2900 deaths, the oldest age cohort did not have a higher excess death rate than the middle age cohort, and the excess death rate actually decreased with deprivation status. Moreover, Iceland had among Europe’s highest excess death rates during the summer, which cannot be attributed to heatwaves. During June, July, and August 2022, comparable southern hemisphere countries furthermore had high excess death rates, which cannot be attributed to heatwaves either, as it was during their winter. Also, Europe’s excess death rate was higher during the 2022–2023 winter than during the 2022 summer, and intuitively not attributed to heatwaves, but neither to cold weather, as that winter was abnormally mild. Finally, the paper discusses the puzzling issue that about 56% more women than men, relative to the population, presumably died from the heatwaves.
Keywords: heatwaves; excess deaths; COVID-19
1. Introduction
During the 2022 summer, Europe experienced several heatwaves with record-breaking temperatures [1], surpassing the one in 2003 [2]. The first began around mid-June 2022 [2], particularly affecting the Iberian Peninsula, France, and Italy [1] with weekly temperature anomalies between +0.78 and +2.33 °C [2]. The second was at its most severe around mid-July [2], extending into the UK, reaching above 40 °C for the first time recorded there [1], and with weekly temperature anomalies between +0.18 and +3.56 °C [2]. The third affected most of Europe throughout August [1], with weekly temperature anomalies between +0.91 and +2.67 °C [2].
Ballester, Quijal-Zamorano, Méndez Turrubiates, Pegenaute, Herrmann, Robine, Basagaña, Tonne, Antó, and Achebak [1] have argued that the heatwaves caused about 62,000 deaths between May 30 and September 4 in Europe. During the same period, the total number of excess deaths on the continent was about 137,000 [3], considerably higher than the 71,000 excess deaths during the 2003 summer [4], indicating that the heatwaves were a strong contributor. However, not ruling out that explanation entirely, this paper’s objective is to address arguments countering the assumption that the heatwaves were a strong cause of deaths, and its outline is as follows. First, as background information, it presents data regarding European excess- and COVID-related deaths before, during, and after the 2022 summer heatwaves. Next, it discusses presumed heat-related deaths in light of data from various sources and countries. Also, it discusses the puzzling issue that about 56% more women than men, relative to the population, presumably died from the heatwaves [2]. The paper concludes by calling for research regarding alternative explanations for excess deaths and suggests potential avenues that may be fruitful.
2. Arguments and Discussion in Light of Statistics from Various Sources
2.1. European Excess- and COVID-Related Deaths
Figure 1 shows European weekly excess deaths in percentages (blue color graph) and weekly smoothed COVID-related deaths per one million (red color graph). These graphs were calculated using data from Our World in Data [3], as explained below. For most weeks, there were data from 32 European countries, the EU, the EFTA (European Free Trade Association), and the UK (for some weeks, a few countries had missing data). The Ballester et al. [2] study, arguing that the 2022 summer heatwaves caused about 62,000 deaths, included 35 countries, but this paper excluded Albania, Montenegro, and Serbia, as Our World in Data [3] provided limited data on those countries.
To measure European weekly excess deaths (blue color graph), this study used weekly country-level excess deaths averages weighted by each country’s population size. Weekly country-level excess deaths, as reported by Our World in Data [3], are the ratio of the actual number of a country’s deaths in a specific week to an estimate of the expected number of deaths in that same country in the same week minus one and multiplied by 100. To calculate the expected number of deaths in a given country in a specific week from 2020 and later, Our World in Data [3] applied regression estimates from pre-COVID historical data between 2015 and 2019, capturing both linear and weekly trends. According to Karlinsky and Kobak [5] (p. 14), this approach captures “both seasonal variation in mortality and a yearly trend over recent years due to changing population structure or socio-economic factors”.
Weekly European COVID-related deaths per one million were also measured by taking the weekly country-level average, as reported by Our World in Data [3], weighed by each country’s population size. (The Introduction stated that the total number of excess deaths between 30 May and 4 September 2022 was about 137,000. This number was attained by calculating accumulated excess deaths in the described data by the week ending on September 4 minus accumulated deaths by the week ending on 29 May).
Figure 1 shows a positive excess death ratio or rate for most weeks from the beginning of the COVID-19 pandemic in 2020 until 2023. During the 2022 summer heatwaves, marked with green reference lines between the week ending on 5 June and the week ending on 4 September, the excess death rate increased at the beginning and decreased at the end. During the same period, there was a modest uptick in COVID-related deaths, but as the increase was low compared to previous ones, it was not a reasonably strong cause of excess deaths during the heatwaves (there appears to be a time lag in COVID-related deaths compared to excess deaths throughout the whole period, which may be due to a delay in reporting). Also, heatwaves or other potential causes of excess deaths may have caused vulnerable people to die of COVID-19.
The pattern of heat-related deaths reported by Ballester et al. [2] (p. 1860) coincides with the pattern of excess deaths in Figure 1 and also correlates with extreme temperatures, both geographically (p. 1863) and over time (p. 1860). Considering these issues alone, one may assume that the heatwaves strongly contributed to excess deaths during the 2022 summer. However, this paper addresses several arguments below that counter that conclusion’s likelihood.
2.2. Presumed Heat-Related Deaths in Light of Data from Various Sources
2.2.1. Age
If the 2022 summer heatwaves were a strong cause of excess deaths, one would assume that the elderly were relatively likely to die, which was also reported by Ballester et al. [2] (p. 1861). However, in England, where the 2022 summer heatwaves were claimed to have caused about 2900 deaths (about 3500 in the UK, according to Ballester et al., [2] (p. 1861)), the oldest age cohort did not have a higher excess death rate than the middle age cohort, according to official data [6]. Specifically, from the week ending on 10 June to 2 September, excess death rates were as follows: for those 85 years or older, 15.0%; aged 75–84 years, 11.5%; 65–74 years, 11.3%; 50–64 years, 16.5%; 25–49 years, 11.0%; and 0–24 years, 11.1% (calculated from the Excel file provided by the UK Office for Health Improvements and Disparities, [6]). These data stand in stark contrast to Ballester et al. [2] (p. 1862) reporting that compared to the youngest age cohort (0–64 years), one hundred times more people died from the heatwaves in the oldest age cohort (80 years and over), and ten times more died in the second oldest age cohort (65–79 years) (the numbers of deaths for these three age cohorts were 16, 160, and 1684 per one million, respectively). Granted, older people are relatively likely to die, which, as they are more vulnerable than young people, particularly would lead to more deaths among them if the heatwaves were the cause. However, as the excess death rates did not deviate substantially across age cohorts, the exponential increase in deaths with age cannot be attributed to the heatwaves, this paper argues.
2.2.2. Deprivation Status
Similar to age, one may also assume that deprived people were relatively likely to die from the heatwaves, as they have fewer resources to protect themselves (e.g., limited access to air-conditioning), are relatively prone to be employed in outdoor manual work, and have relatively low health status at the outset. However, according to official data from the UK Office for Health Improvements and Disparities [6], from the week ending on 10 June to 2 September, the excess death rate in England actually decreased with increasing deprivation status. Specifically, the excess death rate was 15.7% among the least deprived (IMD 5), 15.2% among the second least deprived (IMD 4), 13.6% among the third least deprived (IMD 3), 12.1% among the fourth least deprived (IMD 2), and 10.3% among the most deprived (IMD 1) (calculated from the Excel-file provided by the UK Office for Health Improvements and Disparities, [6]). In other words, the official UK statistics show the opposite of what one would expect concerning the potential association between deprivation status and excess deaths during the 2022 summer heatwaves.
2.2.3. Iceland
During the 2022 summer, Iceland had one of Europe’s highest excess death rates, which reached 36.2% in July, second only to Spain’s, at 39.6% [7]. As Iceland has one of Europe’s lowest summer temperatures, which was actually 0.43 °C below the baseline climatological value that summer [2] (p. 1858), heatwaves were unlikely to have caused excess deaths there.
2.2.4. Southern Hemisphere Countries
During June, July, and August 2022, southern hemisphere countries fairly comparable to Europe also had excess deaths, e.g., rates higher than 20% in Chile in July [3]. Excess death rates were lower but still positive in Brazil, South Africa, Argentina, and Uruguay [3]. These rates cannot likely be attributed to heatwaves, as it was winter in those countries. (Also, the southern hemisphere countries Australia and New Zealand had excess deaths during the same period, but they coincided with an uptick in COVID-related deaths [3]).
2.2.5. The 2022–2023 European Winter
Returning to Figure 1, one can observe that Europe’s excess death rate was higher during the 2022–2023 winter than during the 2022 summer. These winter rates, intuitively, cannot be attributed to heatwaves, but neither to cold weather, as between December 2022 and January 2023, Europe had the second highest temperatures on record [8]. Having said that, The Economist [9] has argued that an increase in energy prices was the cause; however, Iceland, with one of Europe’s lowest electricity prices [10], had an excess death rate of 30.6% in December 2022 [7], Europe’s second highest, and in England, the excess death rate was consistent across deprivation statuses and age cohorts during the winter [6]. (Concerning England, one would assume that the deprived and elderly were more vulnerable to increased energy prices, which was apparently not the case. Also, note that the excess death rate was measured compared to pre-COVID data for similar periods).
2.2.6. The 2022 US Summer Heatwaves
The US, too, experienced numerous record temperatures during the 2022 summer [11], which caused 136 deaths according to official data [12]. Despite the US data potentially being underestimated and the diverging geographic context between the continents, 136 deaths nonetheless stand in stark contrast to Ballester et al. [2] reporting about 62,000 heat-related deaths in Europe. Considering this information with the above arguments makes it reasonable to assume that the European data were overreported, one can argue.
2.2.7. About 56% More Heatwave-Related Deaths among Women Than Men
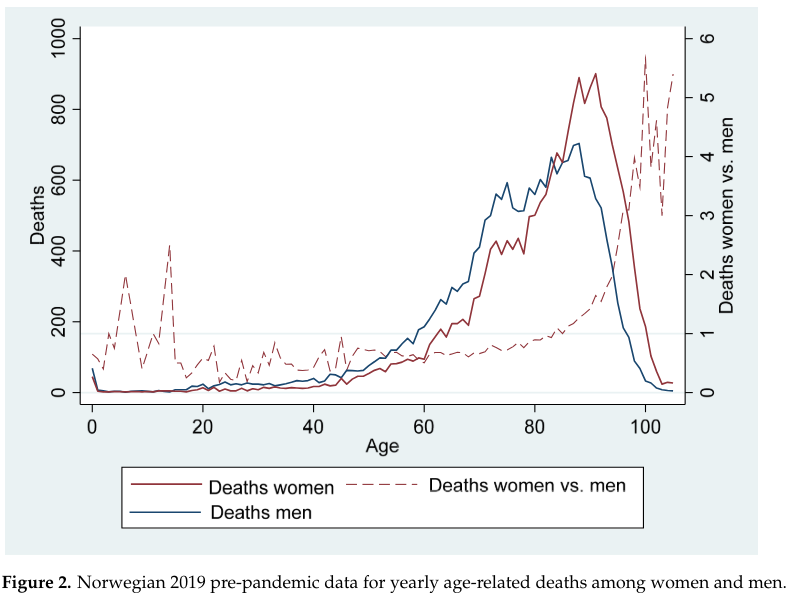
Ballester et al. [2] (p. 1861) reported that about 56% more women than men relative to the population presumably died from the 2022 summer heatwaves, and the difference is significant when considering the reported 95% confidence intervals. Also, they refer to other research addressing a similar pattern (e.g., [13]), but this paper nonetheless finds it puzzling that women, ceteris paribus, were more likely to die from the heatwaves than men. However, an explanation of this reportedly high number is to juxtapose Ballester et al.’s [2] claim that the heatwaves had an exponential mortality effect on the aged (cf. Section 2.2.1) with the fact that more elderly die than young and that among the elderly more women die than men, illustrated in Figure 2 (calculated by the author using data from Statistics Norway, [14]). Hence, one can argue that the reportedly high share of heatwave-related deaths among women was due to Ballester et al. [2] claiming exponential growth caused by age coinciding with more aged women dying than men. (Section 2.2.1 argued that an exponential increase in excess deaths among the elderly is incompatible with English data, which do not show higher excess death rates in the oldest age cohort compared to the middle-aged one. Also, from the week ending on 10 June to 2 September, the English excess death rates for women (men) were as follows: for those 85 years or older, 15.2% (14.8%); aged 75–84 years, 12.5% (10.6%); 65–74 years, 9.9% (12.3%); 50–64 years, 16.1% (16.8%); 25–49 years, 8.7% (12.4%); and 0–24 years, 12.3% (10.5%) (calculated from the Excel file provided by the UK Office for Health Improvements and Disparities [6]). i.e., the excess death rates did not deviate substantially between men and women across age cohorts).
3. A Call for Explanations
The Ballester et al. [2] study did not include control variables in their analyses, and this paper, concluding that the heatwaves were not a strong cause of excess deaths in Europe during the 2022 summer, accordingly encourages future research to investigate alternative explanations. For instance, research may investigate if the per capita accumulation of excess deaths affects the future pattern, as high excess death rates in the past, ceteris paribus, induce fewer in the future, and vice versa. In addition, future research should address the extent to which country-level COVID-vaccination hesitance may have affected the excess death rates during different pandemic phases and study reasons for excess deaths in periods of relatively low COVID-related deaths.
As a response to research suggesting that the excess death rate may be attributed to delayed diagnosing and medical treatments in the wake of the COVID-19 pandemic [15], this paper further encourages future research to test if regions’ or countries’ human development index may be an explanatory factor. It suggests including this measure because countries or regions scoring high on the human development index may have had a better potential to cope with delayed diagnosing and medical treatments compared to countries or regions with lower scores.
This study referred to the 2003 European summer heatwaves that caused about 71,000 deaths [4]. Reviewing the data for that period, two issues are worth mentioning. First, concerning France and partly Italy, excess death rates among the oldest age cohorts were negative prior to the August heatwave, which arguably, at least to some extent, explains the high death rates for similar age cohorts during its occurrence [4] (p. 176). Second, still concerning France and Italy, the relatively high mortality among women [4] (p. 176) was similar to what Ballester et al. [2] reported, which this paper has discussed in detail (Section 2.2.7). Having said that, future research should nonetheless aim to further address potential causes of the excess death rate during the 2003 European summer.
As this paper has argued that neither the 2022 summer heatwaves nor high energy prices during the 2022–2023 winter were strong explanations for excess deaths, hopefully, there can be a fruitful debate about other causes of Europe’s positive trend, even after a decrease in COVID-related deaths (cf. discussion in Section 2.1 related to Figure 1). From this study’s point of view, that is the most constructive path forward in researching one of the most pressing unresolved puzzles concerning human health today.
Funding
This research received no external funding.
Data Availability Statement
All data are from publically available sources.
Conflicts of Interest
The author declares no conflicts of interest.
References
Copernicus Climate Change Service. Extreme Heat. Available online: https://climate.copernicus.eu/esotc/2022/extreme-heat#:~:text=The%20heatwave%20in%20May%20was,than%20typical%20summer%20maximum%20temperatures (accessed on 1 March 2024).
Ballester, J.; Quijal-Zamorano, M.; Méndez Turrubiates, R.F.; Pegenaute, F.; Herrmann, F.R.; Robine, J.M.; Basagaña, X.; Tonne, C.; Antó, J.M.; Achebak, H. Heat-related mortality in Europe during the summer of 2022. Nat. Med. 2023, 29, 1857–1866. [Google Scholar] [CrossRef] [PubMed]
Our World in Data. Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 24 January 2024).
Robine, J.-M.; Cheung, S.L.K.; Le Roy, S.; Van Oyen, H.; Griffiths, C.; Michel, J.-P.; Herrmann, F.R. Death toll exceeded 70,000 in Europe during the summer of 2003. C. R. Biol. 2008, 331, 171–178. [Google Scholar] [CrossRef] [PubMed]
Karlinsky, A.; Kobak, D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. eLife 2021, 10, e69336. [Google Scholar] [CrossRef] [PubMed]
GOV.UK. Office for Health Improvements and Disparities. Excess Mortality in England. Available online: https://app.powerbi.com/view?r=eyJrIjoiYmUwNmFhMjYtNGZhYS00NDk2LWFlMTAtOTg0OGNhNmFiNGM0IiwidCI6ImVlNGUxNDk5LTRhMzUtNGIyZS1hZDQ3LTVmM2NmOWRlODY2NiIsImMiOjh9 (accessed on 3 March 2024).
Eurostat. Excess Mortality by Month. Available online: https://ec.europa.eu/eurostat/databrowser/view/DEMO_MEXRT__custom_1210067/bookmark/table?lang=en&bookmarkId=fc27a3a9-082b-461d-830b-a4c7b36caf4f (accessed on 20 February 2024).
Copernicus Climate Change Service. Copernicus: 2023 is the Hottest Year on Record, with Global Temperatures Close to the 1.5 °C Limit. Available online: https://climate.copernicus.eu/copernicus-2023-hottest-year-record#:~:text=European%20winter%20(December%202022%20%E2%80%93%20February,the%20fifth%2Dwarmest%20on%20record (accessed on 8 March 2024).
The Economist. Expensive Energy may have Killed more Europeans than COVID-19 Last Winter. Available online: https://www.economist.com/graphic-detail/2023/05/10/expensive-energy-may-have-killed-more-europeans-than-covid-19-last-winter (accessed on 10 May 2023).
Statista. Electricity Prices for Households in Iceland from 1st Quarter 2012 to 1st Quarter 2023. Available online: https://www.statista.com/statistics/643385/electricity-prices-for-households-in-iceland/#:~:text=In%20Iceland%2C%20electricity%20prices%20for,bills%20from%202020%20until%202022 (accessed on 11 March 2024).
Axios. Hundreds of Temperature Records Broken as Heat Wave Scorches the U.S. Available online: https://www.axios.com/2022/07/24/heat-wave-temperature-records# (accessed on 11 March 2024).
National Centers for Environmental Information. Billion-Dollar Weather and Climate Disasters. Available online: https://www.ncei.noaa.gov/access/billions/events/US/2022?disasters[]=drought (accessed on 11 March 2024).
Achebak, H.; Devolder, D.; Ballester, J. Heat-related mortality trends under recent climate warming in Spain: A 36-year observational study. PLoS Med. 2018, 15, e1002617. [Google Scholar] [CrossRef]
Statistics Norway. 10325: Døde, Etter Kjønn og 1-Årige Aldersgrupper 1986–2022. Available online: https://www.ssb.no/statbank/table/10325/ (accessed on 12 March 2024).
Pearson-Stuttard, J.; Caul, S.; McDonald, S.; Whamond, E.; Newton, J.N. Excess mortality in England post COVID-19 pandemic: Implications for secondary prevention. Lancet Reg. Health-Eur. 2024, 36, 100802. [Google Scholar] [CrossRef] [PubMed]