Persistent all-cause excess mortality in Norway, particularly among the young, merits an unbiased explanation
Paper rejected for publication in the Scandinavian Journal of Public Health. Below you can read the decision letter from the Editor-in-Chief, Prof. Terje A. Eikemo.
A recent study by White and colleagues reported persistent all-cause excess mortality in Norway from 2022 to 2024, and across all age groups from 2023 to 2024. The study addressed COVID-19 infection as a plausible explanation, but there is another that it did not mention, which I argue in this short communication merits unbiased attention.
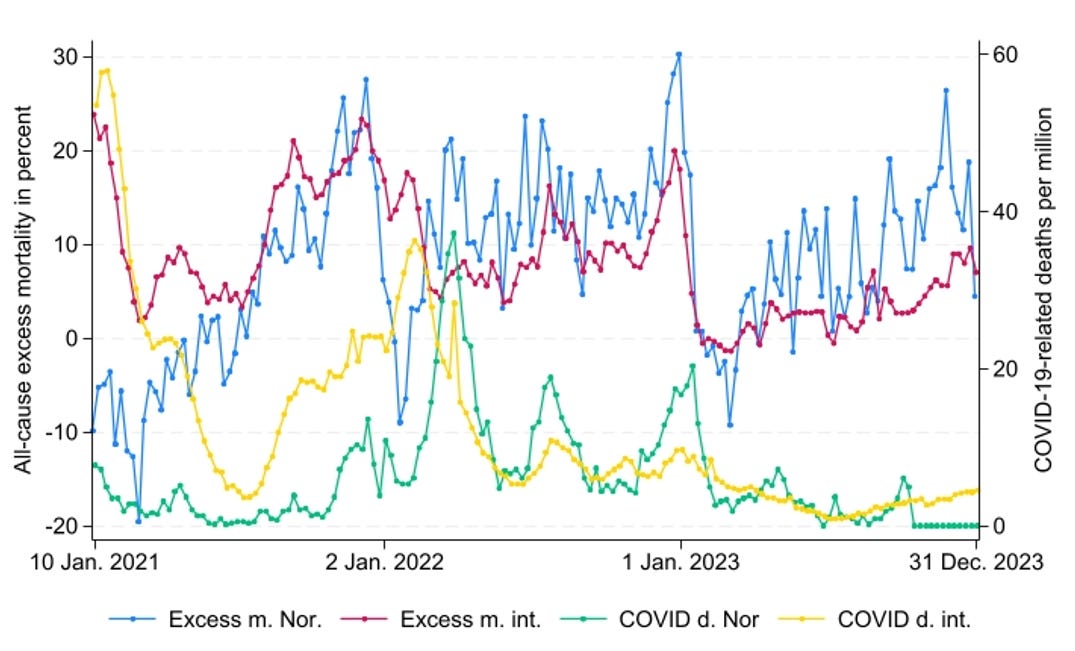
Figure 1 displays weekly all-cause excess mortality and COVID-19-related deaths per million in Norway and 39 high-income countries between 2021 and 2023, from which Our World in Data, the source used, provided consistent data. The 39 countries are EU members, plus Norway, Iceland, Switzerland, the UK, Montenegro, Canada, the USA, Chile, Australia, New Zealand, South Korea, and Israel (data omitted after October 7, 2023). All-cause excess mortality, consistently measured over time and across units, is “the ratio of the actual number of a country’s deaths in a specific week to an estimate of the expected number of deaths in that same country in the same week minus one and multiplied by 100”. Our World in Data applied regressions on 2015-2019 calculations, capturing linear and weekly baseline trends, accounting for “seasonal variation in mortality and a yearly trend over recent years due to changing population structure or socio-economic factors”. COVID-19-related deaths per million is the seven-day smoothed average. The analyses from the 39 countries included averages weighted for each country-unit’s population size.
Figure 1. All-cause excess mortality and COVID-19-related deaths per million in Norway and 39 high-income countries.
In Norway, positive excess mortality in most weeks since mid-2021 (marked in blue) may be due to an increase in COVID-19-related deaths (marked in green), likely caused by the Omicron variant. However, what, at least partly, counters the explanation is that COVID-19-related deaths increased after the excess mortality uptick. Moreover, excess mortality remained consistent after COVID-19-related deaths decreased early in 2022, which further counters the explanation. Considering the 39 countries combined (excess mortality marked in red and COVID-19-related deaths marked in yellow), the pattern since mid-2021 was similar, except that the uptick in excess mortality and COVID-19-related deaths showed a relatively synchronized pattern during the second half of that year, but diverged afterward.
Taken together, COVID-19-related deaths appear to have had a limited effect on all-cause excess mortality since mid-2021in Norway and the 39 countries analyzed combined, and particularly since early 2022. In light of the observed patterns in Figure 1, it is also worth noting that among “530 in-hospital deaths, registered as COVID-19 deaths, in seven hospitals in Athens during the Omicron wave, 240 (45.28%) were reassessed as not directly attributable to COVID-19”.
According to White and colleagues, there may nonetheless be long-term mortality effects from COVID-19 infection not captured by the COVID-19-related deaths observed in Figure 1. However, concerning the high excess death rate, particularly among young people, long COVID is most prevalent among those with comorbidities, and here, older people are in the majority.
Another explanation, not mentioned by White and colleagues, may instead be the COVID-19 vaccine, which I address in the following section. Specifically, I will argue that the vaccine has increased all-cause excess mortality among the population as a whole, and young people in particular.
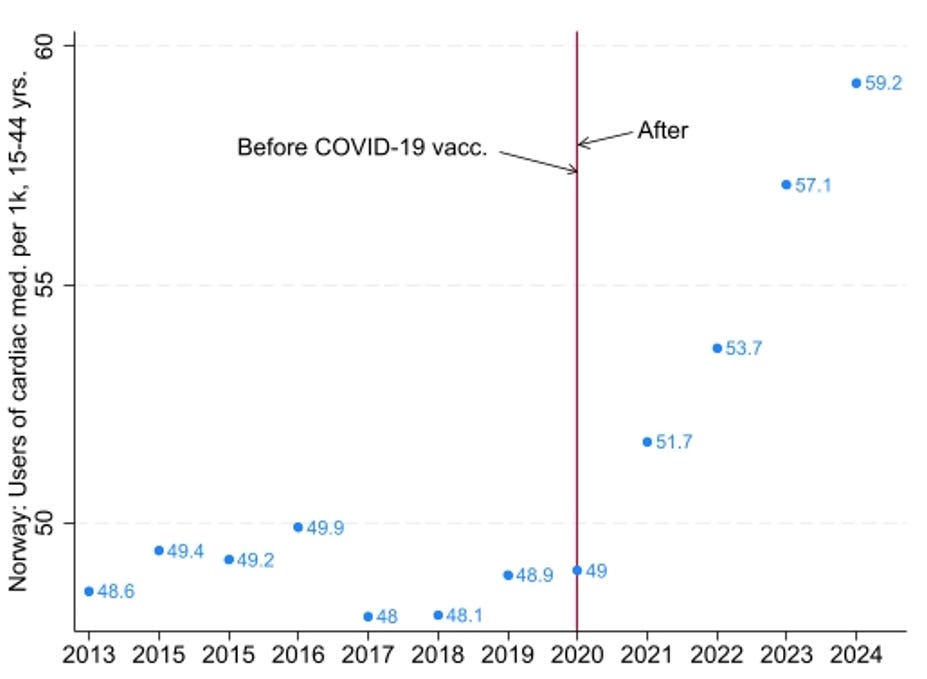
It is now well acknowledged that the COVID-19 vaccine increases the risk of myocarditis in young people, as shown in a large-scale Nordic study, and the finding is echoed by a steady increase in the use of cardiac medication (class C, heart and circulatory system) among young people in Norway, 15-44 years old, reported in Figure 2. The increase began in 2021, coinciding with the COVID-19 vaccine rollout to the younger population from that summer. There was no increase in 2020, which aligns with an Israeli study that found no association between myocarditis and COVID-19 infection before the vaccine rollout. In line with that finding, I have argued that the COVID-19 vaccine has caused far more myocarditis among young people than the virus itself.
Figure 2. Users of cardiac medication per 1000, 15-44 years, in Norway.
As myocarditis can be fatal, also in a long-term perspective, I do not rule out that the COVID-19 vaccine has increased mortality among young people in Norway. Beyond cardiovascular issues, research has further uncovered numerous serious side effects of the COVID-19 vaccine, and randomized trials have shown similar patterns. The side effects may be echoed in research showing that among young people in England aged 12-29, “deaths increased significantly (95 % CIs) in 10 of 11 weeks after COVID-19 vaccination compared to the first week”, and doubled in three. The side effects may also be echoed in other research showing a robust positive association between countries’ COVID-19 vaccination uptake and all-cause excess mortality from March 2022 to December 2023, even after controlling for alternative explanations.
The latter reported study is not yet peer-reviewed, but the conclusion nonetheless aligns with other research I have reported on, along with Japanese scholars arguing that repeated COVID-19 vaccination has led to a significant increase in excess mortality. Therefore, COVID-19 vaccination is not an unlikely explanation for all-cause excess mortality, including among the young, in Norway and elsewhere.
As a response to the British Medical Journal showing bias in covering the COVID-19 pandemic, Kasper and colleagues argued that “[s]cientific journals have a responsibility to be balanced, objective and factual, giving that endorsement of specific ideological or political positions may distort evidence and lead to polarisation of the scientific community and loss of trust.” Hoping that similar bias is to be avoided throughout the medical research literature, including the Scandinavian Journal of Public Health, I share their view.
Decision letter by the Editor
02-Oct-2025
Dear Professor Jarle Aarstad:
(cc: editor of White’s article [Bjørn Heine Strand])
I write you in regard to manuscript SPUB-RI-2025-0400 entitled “Persistent all-cause excess mortality in Norway, particularly among the young, merits an unbiased explanation” which you submitted to the Scandinavian Journal of Public Health.
Thank you very much for your submission and for the effort you have put into addressing this important and sensitive topic. After careful consideration, we are unable to accept your article. The reasoning behind this decision rests on several points.
First, your article does not directly address the commentary by White and colleagues, whose main focus is on the modelling approach and reference years (pre-pandemic versus 2023) used by NIPH (FHI). Your line of argument diverges from theirs and therefore does not engage sufficiently with the piece you intended to comment on.
Second, while you suggest that excess all-cause mortality can be explained by the vaccine, the data presented does not convincingly demonstrate this. The studies you reference speak to vaccine-related mortality from specific causes, age groups, and regions, but to extend this to excess all-cause mortality in Norway requires a much stronger demonstration—showing how these selected causes add up to overall mortality trends, while also taking into account the lives saved by vaccination.
Third, I would advise against framing arguments in terms of bias, as this risks implying that studies or journals which present different conclusions are not objective. The Scandinavian Journal of Public Health is committed to balanced, factual, and evidence-based scholarship. We do not take positions based on ideology, and if robust evidence were presented showing that vaccines contributed to excess all-cause mortality, we—and indeed leading journals such as The Lancet—would certainly consider such work.
I would encourage you, however, to continue developing your analysis. A stronger focus on commenting directly on existing studies (for example, reference no. 7) and highlighting mortality trends within specific causes of death, age groups, or regions would be a valuable contribution. Such an approach may allow you to build a more convincing argument that can fit within the journal’s scope and scholarly dialogue.
We sincerely hope you will consider refining your work and submitting again in the future, whether to the Scandinavian Journal of Public Health or elsewhere. Your engagement with these issues is appreciated, and we encourage you to keep pursuing this line of inquiry.
Thank you again for considering Scand J Public Health for your paper.
With best regards,
Sincerely,
Prof. Terje A. Eikemo
Editor-in-Chief, Scand J Public Health